![]()
heritage
Dyshidrotic eczema is a kind of eczema (dermatitis) of unknown result in that is characterized through a pruritic vesicular eruption on the fingers, palms, and soles. The situation affects teenagers and adults and could also be acute, recurrent, or persistent. A extra appropriate term for this vesicular eruption is pompholyx, because of this bubble. The medical route of dyshidrotic eczema can range from self-limited to chronic, extreme, or debilitating. The situation's unresponsiveness to treatment can be frustrating for the patient and physician (see the photographs beneath). (See clinical.)

irritating vesicles and bullae on the palm. Courtesy of Norman Minars, MD, college of Miami, division of Dermatology & Cutaneous surgical operation.

more than one irritating vesicles on the palm.
Some imagine the terms pompholyx and dyshidrosis are obsolete and favor a new time period, reminiscent of "acute and recurrent vesicular hand dermatitis." The etiology of dyshidrotic eczema is unresolved and is believed to be multifactorial. Dyshidrotic eczema is thought to be to be a response sample resulting from quite a lot of endogenous conditions and exogenous components. (See Etiology.)
complications
Secondary bacterial an infection of dyshidrotic eczema vesicles or bullae can result in cellulitis, lymphangitis, and septicemia (rare). Dystrophic nail changes may boost, with the incidence of transverse ridging, thickening, discoloration, and pitting. Dyshidrotic eczema has no associated mortality, although some severe circumstances can turn into debilitating. (See scientific.)
Prognosis
Dyshidrotic eczema follows a continual, intermittent route, with fewer episodes occurring after heart age. Some mildly affected patients expertise spontaneous resolution within 2-three weeks. (See Epidemiology, therapy, and medications.)
patient schooling
tutor dyshidrotic eczema sufferers to keep away from contact with certain allergens or irritants (eg, nickel), to observe a hand care events that avoids irritants, and to use emollients ceaselessly. as well as, inform folks with this dysfunction concerning the difficulty of attaining a hit therapy. For patient training information, see the pores and skin prerequisites and beauty center, in addition to Eczema (Atopic Dermatitis). (See therapy and drugs.)
Severity index
The Dyshidrotic Eczema space and Severity Index was developed in keeping with severity grades for the number of vesicles per square centimeter, erythema, desquamation, itch, and the extent of affected areas.[1] The index was once found to be a easy standardized way for assessing the situation and used to be used to check disease severity and treatment effectiveness in 2 scientific research. further analysis with higher affected person teams is needed.
NextEtiology
The speculation of sweat gland dysfunction has been disputed because vesicles have not been shown to be related to sweat ducts. A 2009 case document equipped clear histopathologic proof that sweat glands don't play a job in dyshidrosis.[2] however, hyperhidrosis is an disturbing think about forty% of sufferers with dyshidrotic eczema. development in pruritus, erythema, vesicles, and hand dermatitis with fewer or no signs of relapse has been acquired after botulinum toxin A injection.[3]
Dyshidrotic eczema is also related to atopy and familial atopy. Of sufferers with dyshidrosis, 50% have atopic dermatitis.
Exogenous factors (eg, contact dermatitis to nickel, balsam, cobalt; sensitivity to ingested metals; dermatophyte an infection; bacterial infection) may just trigger episodes. These antigens may just act as haptens with a selected affinity for palmoplantar proteins of the stratum lucidum of the epidermis. The binding of these haptens to tissue receptor web sites may just provoke pompholyx.
evidence displays that the ingestion of metallic ions comparable to cobalt can result in type I and type IV hypersensitivity reactions. in addition, they are able to also act as strange haptens, activating T lymphocytes through human leukocyte antigen–unbiased pathways, inflicting systemic allergic dermatitis in the form of dyshidrotic eczema.[4, 5]
Emotional stress[6] and environmental factors (eg, seasonal adjustments, hot or chilly temperatures, humidity) reportedly exacerbate dyshidrosis. as well as, dyshidrosislike eczematous eruptions with using intravenous immunoglobulin infusions were suggested.
Dyshidrosislike eczematous eruptions with using intravenous immunoglobulin (IVIG) infusions had been said. A recent search of the literature recognized pompholyx as one of the vital essential cutaneous adverse results of IVIG, being present in sixty two.5% of the sufferers reported, with seventy five% of those patients creating the lesions after just one IVIG therapy.[7] The eruption tends to be gentle and to wane over time. It usually responds very smartly to topical steroids, but could turn out to be recurrent and more aggressive after repeated doses of IVIG.
In some patients, a distant fungal an infection can result in palmar pompholyx as an identity reaction. in a single study, one third of pompholyx occurrences on the fingers resolved after therapy for tinea pedis. The components believed to be associated with dyshidrotic eczema are mentioned in additional element beneath.
Genetic factors
Monozygotic twins were affected simultaneously by using dyshidrotic eczema. The pompholyx gene has been mapped to band 18q22.1-18q22.three in the autosomal dominant type of familial pompholyx.[8]
Mutations on the filaggrin gene leading to lack of filaggrin, a structural protein of the stratum corneum involved in the barrier operate of the pores and skin, causes dyskeratinization, elevated transepidermal water loss, and an increase in the transepidermal antigen switch. combined, these features have been related to the development of icthyosis and atopic dermatitis, and they is also involved in the construction of irritant and allergic contact dermatitis, which can be well-known stipulations related to dyshidrotic eczema. persistent hand dermatitis, together with dyshidrotis eczema, has additionally been associated with defects within the skin barrier, and, in just a few circumstances, it has been additionally associated with mutations within the filaggrin gene; on the other hand, these have no longer reached statistical importance.[9]
Atopy
As many as 50% of patients with dyshidrotic eczema have reportedly had personal or familial atopic diathesis (eczema, asthma, hay fever, allergic sinusitis). The serum immunoglobulin E (IgE) degree often is increased, even in patients who do not document a private or familial history of atopy. once in a while, dyshidrotic eczema is the primary manifestation of an atopic diathesis.
Nickel sensitivity
this may be a major factor in dyshidrotic eczema. Nickel sensitivity was once reportedly low in some studies of dyshidrosis sufferers, however significantly improved in different studies. elevated nickel excretion in the urine has been stated throughout exacerbations of pompholyx. Ingested metals have been found to impress exacerbations of pompholyx in some patients.
Low-nickel diets have reportedly decreased the frequency and severity of pompholyx flares. A excessive palmoplantar perspiration rate has been suggested to lead to an area focus of steel salts that can provoke the vesicular response. Contact hypersensitivity has been documented in 30% of patients with dyshidrotic eczema.
Cobalt sensitivity
The oral ingestion of cobalt manifests systemic allergic dermatitis as dyshidrotic eczema less incessantly than does the oral ingestion of nickel. much more standard is the simultaneous occurrence of nickel and cobalt hypersensitive reaction considered in 25% of nickel-delicate patients growing pompholyx. In these circumstances, the eczema is frequently more severe. When suspected as the cause of the dyshidrotic eczema, excessive oral ingestion of cobalt should be taken in consideration, whatever the patch take a look at results.[4]
a point-based, low-cobalt weight loss program has been proposed to help patients restrict cobalt ingestion and to keep the serum stage below the brink for growing flares, which is roughly lower than 12 mcg/d. This eating regimen has tested higher compliance than an avoidance eating regimen record. as well as, this weight loss program reduces the quantity of nickel consumed.[4]
exposure to sensitizing chemical substances or metals
Dyshidrotic eczema outbreaks are infrequently associated with exposure to sensitizing chemical compounds or metals (eg, chromium, cobalt, carba combine, scent mix, diaminodiphenylmethane, dichromates, benzoisothiazolones, paraphenylenediamine, perfumes, fragrances, balsam of Peru, Primula plant).
identity reaction
Controversy surrounds the that you can think of existence of an identification reaction, which is thought to be to be a distant dermatophyte infection (tinea pedis, kerion of scalp) triggering a palmar pompholyx reaction (also termed pompholyx dermatophytid).
Fungal an infection
Pompholyx occasionally resolves when a tinea pedis infection is treated, then relapses when the fungal an infection recurs, helping the existence of this reaction sample. Of sufferers who have a vesicular reaction to intradermal trichophytin trying out, less than one third have experienced a resolution of pompholyx after remedy with antifungal dealers.
Emotional stress
this is a that you can think of factor in dyshidrotic eczema. Many patients file recurrences of pompholyx all over worrying sessions. development of dyshidrotic eczema using biofeedback ways for stress reduction helps this speculation.
different factors
isolated experiences describe other imaginable causative elements, equivalent to aspirin ingestion, oral contraceptives, cigarette smoking, and implanted metals, among others. A 3-year potential find out about of the motives of dyshidrotic eczema (pompholyx) in one hundred twenty patients found motives of pompholyx related to contact publicity (67.5%), together with to cosmetic merchandise (31.7%) and metals (sixteen.7%); interdigital-plantar intertrigo (10%); and internal elements (6.7%), with a further 15% of sufferers having undiagnosed (idiopathic) causes almost definitely related to atopic elements.[10]
Contact hypersensitive reaction was found in 89 (seventy four.2%) of the 120 patients. the most conventional allergens have been nickel, bathe gel, chromium, heady scent, shampoo, and balsam of Peru. less ordinary allergens have been lanolin, cobalt, thiuram, lauryl sulfate, contemporary tobacco, p -phenylenediamine (PPD), formaldehyde, parabens, and octyl gallate. In 97 of 193 positive patch check outcomes, correlation existed between the appliance of the agent and pompholyx recurrence. The relevance of the analysis was once confirmed in eighty one (sixty seven.5%) of the one hundred twenty sufferers. In abstract, probably the most accepted motives of pompholyx associated to contact with resources had been hygiene product intolerance (forty six.7%), steel hypersensitive reaction (25%), and others (28.3%).
Intertrigo happened in 19 (15.eight%) of the one hundred twenty patients. Of these people, eighty% offered with dermatophytosis and 20% introduced with candidiasis. After three weeks of antifungal remedy, 6 of 19 patients remained symptomatic for pompholyx.
with regard to internal causes, 30 sufferers introduced with a good patch check end result for metals, however handiest 2 presented with exacerbations of the lesions after a challenge take a look at.
Of 58 patients with a historical past of smoking tobacco, 5 offered with a favorable reaction, and 2 of those reactions have been considered relevant. Drug hypersensitive reaction was determined to be the causative agent in three patients (amoxicillin in 2 and intravenous immunoglobulin in 1). food-related pompholyx used to be detected in four sufferers, and, after a challenge take a look at, reactivation came about in three of these sufferers (2 for paprika and 1 for orange juice).
Ultraviolet a mild
In a case collection, 5 patients with prior diagnosis of pompholyx developed lesions morphologically and histologically in step with a vesicular dermatitis after provocation with lengthy-wavelength ultraviolet A (UVA) mild. further workup dominated out contact dermatitis, polymorphic light eruption, and warmth because the perpetrator, confirming that the reaction used to be due to actual photosensitivity reasonably than to photoaggravation.[11]
Pompholyx due to UVA publicity could probably be considered a model of seasonal (summer time) pompholyx. In the us, dyshidrotic eczema is extra recurrently viewed in warmer climates and all the way through the spring and summer months. A learn about in Turkey additionally revealed a higher incidence of dyshidrotic eczema in the summer months.[12]
(Of pastime, UVB phototherapy and photochemotherapy are neatly-identified, efficient treatments for pompholyx.)
PreviousNextEpidemiologyOccurrence in the united states
Dyshidrotic eczema happens in 5-20% of patients with hand eczema and extra often develops in warmer climates and all the way through spring and summer time months (seasonal or summer pompholyx).
global occurrence
Dyshidrotic eczema accounted for 1% of preliminary consultations in a 1-yr Swedish find out about. In a find out about of 107,206 Swedish people, fifty one (0.05%) have been identified with dyshidrosis. Of all hand dermatitis cases in that inhabitants, three% had dyshidrosis.[13]
In a retrospective learn about reviewing information of 714 Portuguese sufferers during a 6-12 months length, Magina et al discovered dyshidrotic eczema to be the 1/3 most typical kind of hand dermatitis (20.3%).[14]
sex- and age-related demographics
The male-to-feminine ratio for dyshidrotic eczema has variably been mentioned as 1:1 and 1:2. Dyshidrotic eczema affects folks aged four-76 years; the mean age is 38 years. the height incidence of the situation occurs in patients aged 20-forty years. After center age, the frequency of dyshidrotic eczema episodes tends to decrease.
PreviousProceed to medical Presentation , Dyshidrotic Eczema
 Hyperpigmented streaks on the dorsa of hands of a patient with bergapten phototoxicity
Hyperpigmented streaks on the dorsa of hands of a patient with bergapten phototoxicity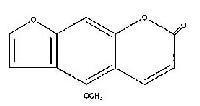 Molecular structure of 5-methoxypsoralen (bergapten) PreviousNextEpidemiologyFrequencyUnited States
Molecular structure of 5-methoxypsoralen (bergapten) PreviousNextEpidemiologyFrequencyUnited States
 irritating vesicles and bullae on the palm. Courtesy of Norman Minars, MD, college of Miami, division of Dermatology & Cutaneous surgical operation.
irritating vesicles and bullae on the palm. Courtesy of Norman Minars, MD, college of Miami, division of Dermatology & Cutaneous surgical operation.  more than one irritating vesicles on the palm.
more than one irritating vesicles on the palm.